
Luis Gruberg, MD, FACC
Presenter: Judith S. Hochman, MD, New York University School of Medicine, New York, NY
Previous studies have shown that prompt and early reperfusion therapy improves left ventricular function and survival in patients presenting with ST-segment elevation myocardial infarction (MI)。 However, approximately one third of all patients do not receive reperfusion therapy for a variety of reasons. The management of these patients, especially with regard to percutaneous recanalization of the infarct-related artery (IRA), has not been elucidated, although there is a strong bias in favor of revascularization. It has been postulated that a patent IRA would attenuate remodeling, increase electrical stability, and provide collaterals to other territories. However, percutaneous coronary intervention (PCI) may actually be harmful in some patients due to periprocedural complications, distal embolization, and the potential for acute reocclusion.
Study Design
The Occluded Artery Trial (OAT) was a multicenter, international study that was designed to test the hypothesis that a strategy of late PCI to open the occluded IRA would reduce the first occurrence of a composite endpoint of death, reinfarction, or New York Heart Association (NYHA) IV heart failure by 25% compared with optimal medical treatment alone.
To be eligible, patients were required to have a confirmed MI with a completely occluded IRA (day 3-28), as well as high-risk criteria (ejection fraction < 50% and/or proximal occlusion of major epicardial vessel supplying > 25% of the left ventricle)。 Major exclusion criteria included left main or triple vessel disease, hemodynamic or electrical instability, rest or low-threshold angina, and NYHA class III-IV heart failure or shock.
Primary endpoint: Composite of death, rehospitalization for NYHA class IV heart failure or MI.
Secondary endpoints:
Results
Between 2000 and 2005, a total of 2166 patients were randomized to either the PCI plus optimal medical treatment arm (n = 1082) or optimal medical treatment alone (n = 1084)。 PCI was attempted in 99% of patients randomized to PCI and medical treatment and in 8.3% of patients in the medical treatment arm. In the PCI arm, 72% of the patients were treated with glycoprotein IIb/IIIa inhibitors, 8.1% with drug-eluting stents, and a non-IRA was treated in 7% of patients. Baseline clinical and angiographic characteristics are shown in Table 1. Medications at discharge are shown in Table 2.
Table 1. OAT: Baseline Characteristics
|
PCI (n = 1082) |
Medical (n = 1084) |
|
|
Clinical
|
||
|
Age (yrs)
|
59
|
59
|
|
Previous MI (%)
|
12
|
11
|
|
Diabetes (%)
|
19
|
23
|
|
NYHA class I (%)
|
83
|
83
|
|
Lytic therapy (%)
|
21
|
18
|
|
Days from MI to randomization
|
8
|
8
|
|
Angiographic
|
||
|
Infarct artery LAD (%)
|
35
|
37
|
|
TIMI flow 0 (%)
|
83
|
83
|
|
Collaterals present (%)
|
83
|
89
|
|
Single vessel (%)
|
82
|
82
|
|
Ejection fraction (%)
|
47
|
48
|
PCI = percutaneous coronary intervention; MI = myocardial infarction; NYHA = New York Heart Association; LAD = left anterior descending
Table 2. OAT: Medications at Discharge
|
PCI (n = 1071) |
Medical (n = 1078) |
|
|
Aspirin (%)
|
97
|
94
|
|
Beta blockers (%)
|
86
|
89
|
|
ACE inhibitor or ARB (%)
|
80
|
80
|
|
Lipid-lowering (%)
|
80
|
82
|
|
Thienopyridine (%)
|
91
|
29
|
PCI = percutaneous coronary intervention; ACE = angiotensin-converting enzyme; ARB = angiotensin receptor blocker
At 5-year follow-up, the primary endpoint of the study (death/MI/congestive heart failure) occurred in 17.2% of patients in the PCI arm vs 15.6% in the medical treatment arm (Figure)。 Individual endpoints of the study were identical in both arms, with the exception of a higher rate of fatal and nonfatal MI in the PCI arm of the study (Figure)。
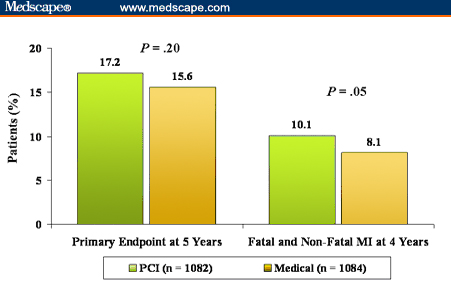
Figure. OAT: clinical outcomes.
Conclusions
Discussant: Robert M. Califf, MD, Duke University School of Medicine, Durham, North Carolina
Dr. Califf acknowledged that OAT was a well-executed study that was managed independent of commercial interests and measured real clinical outcomes. Extrapolating these results to the general population may be difficult, as many sites had very low rates of enrollment, especially in the United States. Dr. Califf questioned whether this study can be generalized to the US practice and population. He also noted that there is some difficulty accounting for evolving technology, as only 8% of patients in OAT were treated with drug-eluting stents.
However, according to Dr. Califf, the take-home message will be that there is no compelling reason to intervene in asymptomatic patients > 24 hours post-MI with a totally occluded IRA.
